AI is turning chest X-rays into predictive health tools: A routine scan may know your health future before you feel it
The Most Familiar Medical Image May Be Hiding the Most Surprising Insight
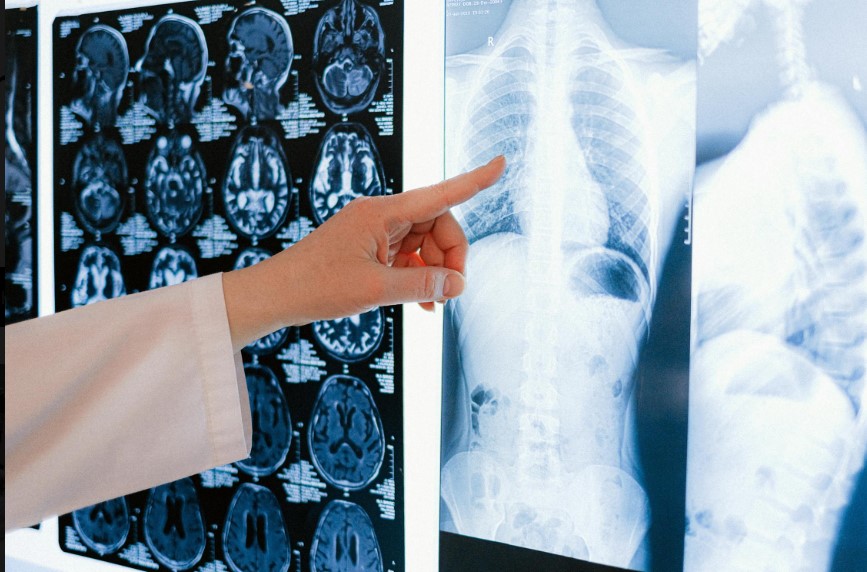
For more than a century, the chest X-ray has been one of medicine’s most routine tools. Doctors glance at it to spot pneumonia, check heart size, or rule out lung collapse. It is fast, inexpensive, and ubiquitous so common that it is rarely considered innovative.
Now, artificial intelligence is turning that humble image into something far more provocative: a window into how fast the human body is aging.
A new study published in The Journals of Gerontology suggests that deep learning models trained on chest X-rays can detect biological aging and early cardiovascular risk with a precision that outperforms some of the most advanced DNA-based aging tests available today. The implications are profound, not only for preventive medicine, but for how we understand aging itself.
Chronological Age vs. Biological Reality
Aging has always been measured by the calendar. But anyone who has spent time in a hospital waiting room knows that two 55-year-olds can look, and function, very differently.
That gap is known as biological age: a measure of how much wear and tear the body has actually accumulated. Until recently, scientists relied on “epigenetic clocks,” which estimate biological age by analyzing DNA methylation patterns. These tools are powerful but expensive, invasive, and difficult to deploy at scale.
The new research suggests that much of this information may already be visible—quietly embedded in routine medical imaging.
Teaching Machines to Read Time in the Body
The study analyzed data from 2,097 adults enrolled in the Project Baseline Health Study, a large, multi-site U.S. initiative designed to track health trajectories over time. Researchers trained a deep learning model, called CXR-Age, on standard chest X-rays, asking it to estimate each participant’s biological age.
The results were striking.
CXR-Age not only predicted age accurately, but also showed strong associations with early signs of cardiopulmonary decline—long before clinical symptoms emerged. These included coronary artery calcium, declining lung function, increased frailty, and elevated blood proteins linked to inflammation and neurodegeneration.
In contrast, widely used DNA-based aging clocks such as Horvath Age and DNAm PhenoAge showed weaker or inconsistent correlations, particularly among middle-aged adults.
In plain terms: the X-ray knew things the genes did not.
Why the Lungs and Heart Tell the Truth
Chest X-rays capture more than anatomy. They reflect cumulative exposure to air pollution, smoking, inflammation, metabolic stress, and cardiovascular strain. These forces shape the body gradually, leaving subtle signatures invisible to the human eye but legible to machine learning models trained on vast datasets.
“Medical imaging captures the lived experience of aging,” one researcher involved in the study noted. Unlike genetic markers, which reflect predisposition, imaging reveals the consequences of life itself.
This distinction matters. Risk does not emerge overnight. It accumulates.
A New Kind of Early Warning System
If validated in broader populations, AI-derived biological age could become one of the most powerful screening tools in modern medicine.
Imagine a routine chest X-ray, already ordered for unrelated reasons, flagging a patient as biologically older than their chronological age. That signal could prompt earlier lifestyle interventions, closer cardiovascular monitoring, or preventive therapies years before disease manifests.
This is not diagnosis. It is anticipation.
Preventive medicine has long struggled with timing. Intervene too early, and costs rise without clear benefit. Intervene too late, and outcomes worsen. Biological age may help bridge that gap.
From Reactive Care to Predictive Medicine
Healthcare systems are built to treat illness, not foresee it. AI models like CXR-Age hint at a different paradigm—one where disease is intercepted during its silent phase.
This shift aligns with broader trends in medicine: precision health, risk stratification, and personalized care pathways. But unlike genetic testing or advanced imaging, chest X-rays are already embedded in clinical workflows worldwide.
That scalability is crucial.
AI does not need new machines. It needs new interpretations.
Ethical and Clinical Guardrails Matter
As with all medical AI, caution is warranted. Biological age is not destiny. Used improperly, it could lead to overtesting, anxiety, or insurance discrimination.
Transparency, validation across diverse populations, and clinician oversight are essential. AI should inform decisions, not replace them.
There is also a deeper philosophical question: how much do we want to know about our future health? Predictive power is only helpful if paired with actionable, humane care.
A Broader Lesson About AI in Healthcare
This study underscores a pattern emerging across medicine: the most transformative AI breakthroughs are not flashy consumer tools, but quiet reinterpretations of existing data.
The future of healthcare innovation may lie less in new sensors and more in learning to read what we already collect, better, earlier, and more holistically.
In that sense, AI is not inventing new medicine. It is uncovering what has been hiding in plain sight.
Aging, Reimagined
A chest X-ray that estimates biological age challenges a deeply held assumption, that aging is abstract, genetic, and slow-moving. Instead, it appears measurable, visible, and responsive to intervention.
That realization carries hope. If aging can be seen earlier, it can be addressed earlier. And if disease risk is detectable before symptoms arise, medicine may finally shift from crisis response to long-term stewardship of health.
The most familiar image in medicine may soon become one of its most predictive.
